FDA Panel Addresses EtO Sterilization
In order to prevent potential shortages of critical medical devices, manufacturers and state regulators must resolve environmental concerns about ethylene oxide (EtO) sterilization. This was the consensus of the U.S. FDA CDRH General Hospital and Personal Use Devices Advisory Committee panel following one-and-a-half days of discussion at a public meeting Nov. 6–7 in Gaithersburg, Md.
The panel urged FDA to take steps to mitigate the risk of shortages, including the possibility of overriding state legislation that has resulted in closures of facilities sterilizing devices using EtO. This would require high-level discussion with the leadership of the U.S. Department of Health and Human Services, the agency that oversees FDA.
The meeting follows two closures of Sterigenics facilities in Illinois and Georgia and the potential closure of a Becton Dickinson site in Georgia (1,2). The issue began in February when the Illinois Environmental Protection Agency issued a state order closing the Sterigenics plant in Willowbrook, Ill. due to concerns about the plant was releasing unsafe levels of EtO into the air (1). A recent bill in the Illinois House seeks to phase out EtO use by medical device manufacturers in the state due to concerns about cancer risks to communities near these facilities (3).
Compounding the issue, the closure of any further EtO sterilization facility is likely to exacerbate existing capacity concerns regarding devices.
Mark Leahy, representing the Medical Device Manufacturers Association (MDMA), offered some sobering statistics. MDMA represents 300 small- to midsize device manufacturers. Ten days prior to the meeting, MDMA surveyed its membership about the impact of further closures. 300 device manufacturers in the ten days prior the meeting.
“94% of respondents said that if their primarily sterilization went offline, they would have to eventually close,” he said. “This is not anything theoretical...for a number of our small companies, the Willowbrook facility was the only place they sterilized their products.”
He pointed out that even if a facility were to switch to an alternative or reduce EtO, even going offline for a short amount of time would cause a negative impact on supply, emphasizing that "the capacity right now in the EtO market is nonexistent."
This has the potential for disastrous outcomes, according to Kara Mascitti, MD, an emergency room physician with St. Luke's University Health Network.
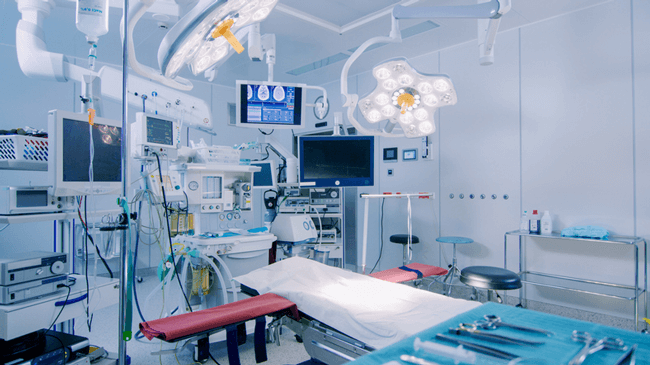
“As an infectious disease physician, I know firsthand the importance that physicians have access to sterilized products for patient care,” she said. “Every single patient that is admitted to one of our hospitals or visits one of our emergency rooms requires at least one sterile product as part of their medical care.”
What is Ethylene Oxide (EtO) Sterilization?
Ethylene oxide (EtO) is a colorless, flammable gas used to sterilize medical devices made from specific materials or have multiple layers of packaging, such as catheters. EtO is often the only method for sterilizing these products without damaging the device during sterilization. According to the FDA website, 50% of all medical devices in the United States are sterilized with EtO.
EtO is also a carcinogen and falls under U.S. Environmental Protection Agency (EPA) regulations. The major concern is around emissions of EtO from plants into the surrounding environment.
Phil Cogdill, Senior Director of Quality, Sterilization Microbiology, Medtronic, expanded on the necessity of EtO and opportunities for device manufacturers to reduce use of it.
“Sterilization is a complex process that starts and ends with the patient,” he emphasized, further explaining that sterilization for devices involves more than just eradicating microorganisms; it also requires ensuring that device functionality or performance is not impaired.
Even more challenging, few of the products currently sterilized with EtO can be sterilized using other methods. At this time, 50% of all devices worldwide are sterilized using EtO. While there are other sterilization methods (moist/dry heat, radiation, hydrogen peroxide, chlorine dioxide, etc.) in addition to ways to reduce EtO emissions (product packaging modifications, optimized processes, reduced exposure times, reduced gas concentrations and more optimized cycles), any changes to sterilization methods or approaches will require time and investment, again, resulting in potential shortages.
To emphasize the complexity of EtO sterilization, Cogdill showcased an oxygenator to show the complexity and the number of materials and components comprising a device. Due to this complexity it would be hard to switch to a different sterilization process, particularly when taking into account the time to develop and validate a new process.
Is This a Job for EPA?
Following the meeting, Cogdill answered some questions for the PDA Letter. While he spoke at an FDA meeting, he thinks this is more of a matter for EPA.
“We definitely want to see the EPA take a leadership role,” he said. “We do understand the ISA regulations [Integrated Science Assessment for ethylene oxide] are currently under review. I believe the medical device industry is looking forward to working with the EPA and reducing the emissions to whatever requirements are provided by the EPA.”
He hopes that any changes to the EPA’s regulations on EtO helps reduce the public “anxiety around this chemical and its use for sterilizing medical devices.”
In fact, he thinks EPA needs to address the state regulations, not FDA.
“I do not think the FDA is the appropriate government agency for that but with these new regulations it is certainly going to help the states to be consistent with the federal position and hopefully that will stop some of the rash bill passing that has been going on other states.”
Gary Socola, President, HIGHPOWER Validation Testing & Lab Services Inc., also took some time to answer a few questions for the PDA Letter. He explained that the crux of the current issues with EtO sterilization lies in changes the EPA made in 2014 to its calculation formula which determines the safe breathing level of EtO. 2014 was the last year EPA performed its National Air Toxics Assessment (NATA), and this data was released earlier this year.
“[FDA] does not have the ability to regulate EtO emissions. That is directly a function of the EPA,” he said.
"A lot of the issues that have occurred have been because of the change that the EPA made with the methodology of how they calculate a safe level of EtO for breathing, and that changed from 2011 to 2014, and I believe a lot of the confusion was because of this change.”
Socola thinks this change alarmed the public, particularly those living near EtO sterilization plants. “Emotions can certainly overrun scientific data and factual information if not reviewed thoroughly,” he said.
When it comes to FDA’s role, Socola would like FDA to prevent device shortages by looking at how the Agency currently responds to drug shortages. He pointed out that FDA has taken on a number of initiatives addressing drug shortages, including a team of staff within CDER responsible for preventing and mitigating drug shortages. Yet the Agency has little information available in the way of medical device shortages--something easily highlighted by a Web search.
“If you typed in ‘FDA’s jurisdiction for drug shortages,’ and then typed in ‘FDA’s jurisdiction for medical device shortages,’ you would notice that there is a significant difference in the amount of information that is available for drug shortages and what the FDA can do during them, as compared to what they can do for medical device shortages,” Socola explained.
Reverberations for Drug Manufacturing
The EtO debate has been primarily a medical device issue but should sterile drug manufacturers be concerned?
“Whenever you are dealing with aseptic manufacturing and sterile drugs, a lot of the ancillary personal protective gear and a number of the equipment that is used with it can be EtO sterilized to help that process, so I would say that there is probably some impact if those sterilizers were to be shutdown,” Cogdill told the PDA Letter.
Socola pointed to drug device combination products as another area that could be impacted.
“There are the delivery devices doing the injections of some of these pharmaceutical drugs,” he said. “Diabetes in itself has a number of different types of medical devices that inject insulin and other types of pharmaceutical solutions. How are those types of devices going to be affected?
FDA, EPA Look Ahead
In addition to researching potential emergency measures to override state legislation, the Advisory Committee came to consensus regarding the following:
- While it is possible to change EtO sterilization cycles or loads to reduce EtO use and also maintain effective sterilization, no single method addresses all issues
- Alternatives to the overkill validation method should be considered by FDA
- Consistent with current standards, FDA should consider moving to a risk-based assessment of sterility assurance levels for some sterilized medical devices
- FDA should encourage manufacturers to look into the possibility of using existing large-scale industrial sterilization modalities to take over a portion of EtO sterilization
- Manufacturers should review which sterilization modalities are potentially compatible with their devices, and, where possible, validate alternate methods
- FDA must continue to collaborate with industrial stakeholders on alternatives to EtO sterilization and adoption of optimized EtO processes that use less EtO and emit less EtO into the environment in the near term
FDA will continue to review the situation around EtO and continues to seek input about alternatives (4). In addition, EPA tentatively expects to come out with proposed rules on EtO sterilization in May 2020 following public hearings this month (4). From the discussion at the Advisory Committee meeting, collaboration between the two agencies is likely, and both Agencies will continue to seek industry input.
[Editor's Note: Read an update from the Jan. 15 hearing on EtO at the U.S. EPA headquarters.]
References
- Sookne, K. “FDA Comments on Potential Device Shortages in the Face of ETO Facility Interruptions/Closures.” Healthcare Packaging (Oct. 25, 2019)
- “BD Statement on Georgia Facilities.” (July 25, 2019)
- Hawthorne, M. “Illinois House approves phaseout of cancer-causing ethylene oxide, but Medline Industries and business groups are working to quash bill in Senate.” Chicago Tribune (Oct. 30, 2019).
- Crotti, N. “Federal agencies will control the fate of medtech’s most-used sterilization method.” Medical Design and Outsourcing (Nov. 15, 2019)


