Effective Strategies for Investigating Media Fill Failures in Sterile Manufacturing
[Editor’s Note: This article was originally published December 6th and taken down December 18th due to the author’s updates of the article.]
Sterile manufacturing is a critical process that requires meticulous attention to detail and adherence to strict aseptic techniques.
One of the key measures to ensure the success of the sterile manufacturing process is the media fill, also known as aseptic process simulation. Media fill exercises should be conducted during the initial setup of an aseptic filling line and periodically thereafter. Manufacturers can identify potential issues, train operators, and implement corrective actions to prevent contamination and ensure product safety by conducting media fill exercises. In cases where a media fill test results in failure, a comprehensive investigation becomes imperative, and there are some effective strategies for investigating media fill failures in sterile manufacturing, as well as clear examples to know when media fill failures are present.
Acceptance Criteria for Media Fill
The acceptance criteria for media fill are defined in regulatory guidelines.
As per Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing, published in September 2004, recommended criteria for assessing state of aseptic line control are as follows:
- When filling fewer than 5000 units, no contaminated units should be detected.
- One contaminated unit is considered the cause for revalidation, following an investigation.
- When filling from 5,000 to 10,000 units:
- One contaminated unit should result in an investigation, including consideration of a repeat media fill.
- Two contaminated units are considered cause for revalidation, following investigation.
- When filling more than 10,000 units:
- One contaminated unit should result in an investigation.
- Two contaminated units are considered cause for revalidation, following investigation.
EU GMP Annex 1: Manufacture of Sterile Medicinal Products, section 9.46 mentions that “The target should be zero growth. Any contaminated unit should result in a failed process simulation and the following actions should occur:
- An investigation to determine the most probable root causes.
- Determination and implementation of appropriate corrective measures.
- A sufficient number of successful, consecutive repeat media fills (normally a minimum of three) should be conducted in order to demonstrate that the process has been returned to a state of control.
- A prompt review of all appropriate records relating to aseptic production since the last successful APS. The outcome of the review should include a risk assessment of potential sterile breaches in batches manufactured since the last successful process simulation. All other batches not released to the market should be included in the scope of the investigation. Any decision regarding their release status should consider the investigation outcome.
- All products that have been manufactured on a line subsequent to a process simulation failure 2236 should be quarantined until a successful resolution of the process simulation failure has occurred.
- Production should resume only after completion of successful revalidation.
Investigating Media Fill Failures
Conducting an investigation into media fill failures is a complex process that requires substantial effort, expertise, and experience. The objective is to accurately pinpoint the root cause of the failure and identify the most relevant corrective and preventive actions. When initiating the investigation, it is crucial to identify the precise moment when the failure occurred. This can be achieved by meticulously monitoring the entire sequence of events during the media fill process and documenting any interventions, activities, and individuals involved.
Establishing Connections Between Activities and Contamination
To effectively investigate isolated instances of contaminated units, it is important to tabulate all activities against the time they were performed. This includes meticulously recording the following:
- Start time of filling assembly
- Filling operation
- Interventions
- Shift changes
- The addition of rubber stoppers (for vials)
- Environmental monitoring
- Breakdowns
- Interventions and actions taken during the media fill process
Once the activities and time points have been documented, it is crucial to establish a connection between these activities and any instances of contamination or failures that may have occurred. By analyzing the records, manufacturers can identify potential factors that contributed to the failures. Furthermore, it is imperative to meticulously record every intervention and action taken during the media fill process. While not mandated by regulatory requirements, video recording can also provide valuable insights into personnel practices that may have a detrimental impact on the aseptic process.
Factors to Consider Regarding Investigation
A more comprehensive investigation becomes necessary if a clear cause is not evident from the initial review. This involves examining these factors:
- Environmental conditions during filling operations
- Air velocity
- High-efficiency particulate air filter integrity (HEPA)
- Cleaning and sanitization issues
- Trends in environmental monitoring results
- Machine maintenance
- System abnormalities
- Proper assembling by trained operators
It is important to revisit the most recent area and equipment requalification, focusing on critical factors such as HEPA filter integrity, air velocity, and particle counts. Any deviations or anomalies in these factors can potentially contribute to media fill failures.
Examples of Possible Reasons for Media Fill Failure
- When sterilizing the filtration skid, a connection or some part of the skid may not be sterilized and was not identified or evaluated during qualification.
- Aseptic connection is done in a Grade C or Grade B environment instead of Grade A due to a lack of procedure or operator awareness.
- Leakage from filling needle during filling operation that results in the repeated intervention of filling needle adjustment and cleaning of a spilled product under Grade A.
- Addition of a new item in autoclave load not part of validated load pattern.
- Addition of a new connection, new attachment like a dip tube, and inert gas purging tube in sterilizing filtration skid, which was not part of the validated system.
- Sterilized vessels are not maintained under positive pressure throughout the sterile filling operation, creating a scope of ingress of non-sterile air in sterilized vessels.
- Validated sterilization parameters are not incorporated in standard operating procedures, creating a possibility of using a non-validated sterilization cycle.
- The inner surface of a sterile holding vessel has dents, scratches, cracks, and rough surfaces, which can support microbial proliferation.
Seven Measures to be Taken to Prevent Media Fill Failure
Section 9.32 of Annex I states that “The Aseptic process simulation should not be considered as the primary means to validate the aseptic process or aspects of the aseptic process. The effectiveness of the aseptic process should be determined through process design, adherence to the pharmaceutical quality system and process controls, training, and evaluation of monitoring data.”
The measures to be considered as a part of routine operation for sterility assurance in day-to-day operation as well as during media fill are described in these seven steps:
1. Well-Defined Procedures for Aseptic Operation
The operating procedure should elaborate in detail every step for aseptic assembling and performing aseptic intervention, highlighting precautions to be taken during critical activities. For example, remove the wrapping of sterilized components using forceps and avoid direct touching of gloves to sterilized items. Ensuring that the sterile component is handled only by sterile tools. Do not lean over exposed sterile components.
2. Operator Training
First time and refresher training and awareness about basic microbiology to operators working in an aseptic environment ensures that operators are constantly made aware of the criticality of aseptic operation. Visual sign boards, videos on critical aseptic operation, and detailed standard operating procedures (SOPs) with photographs in SOPs play vital roles in operator skill development.
3. Validation vs. Routine Operation
The system should be established to ensure that only the validated parameters for critical operations like sterilization are transferred to standard operating procedures, and the quality control unit should ensure it. Any changes to validated load patterns, sterilization-in-place (SIP) skids, and vessels should be done through change control and should be validated.
4. Inspection of Sterile Holding Vessel and Equipment Assembly
The condition of the gaskets in the sterile holding vessel is a crucial factor that can contribute to potential failures. Regular inspection of gaskets used in sterile holding vessels and SIP skids is necessary to ensure they provide the airtight seal and pass the leak test (see Figure 1). The inspection should include checking the integrity of connections, clamps, seals, and view glasses within the sterile holding vessel, filling machine, and product transfer line. A ruptured, damaged gasket can lead to media fill failure.
 Figure 1 Gaskets, clamps, seals, and view glasses for sterile holding vessel
Figure 1 Gaskets, clamps, seals, and view glasses for sterile holding vessel
5. Cleaning of Inner Surfaces and Hidden Contaminants
 Figure 2 A vessel's interior and rough surface example
Figure 2 A vessel's interior and rough surface example
A thorough inspection of the vessel's interior is essential to ensure no residual glue, tape, or other contaminants could create hiding spots for microorganisms during the SIP process. Regular cleaning protocols should include checks for such deficiencies (see Figure 2). Failure to address these issues can result in media fill failures or product contamination.
6. Validating Wrapping and Assembly of Filling Equipment
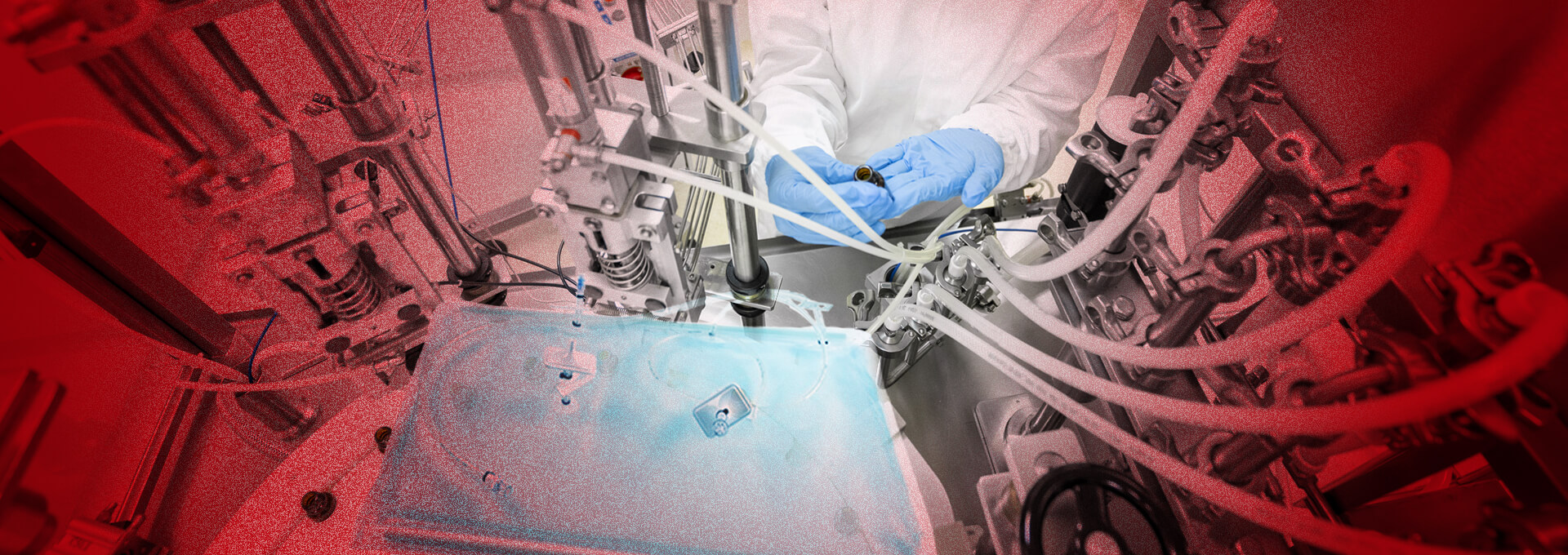
Proper assembly of the filling equipment is crucial to ensure the successful filling of products into vials, ampoules, or pre-filled syringes (see Figure 3). The sterilization of the filling assembly should be validated, and transfers from the autoclave to the filling machine should pass through a mobile laminar airflow unit to prevent contamination. It is important to validate the wrapping of sterilized items, their sterilization process, and the transfer process to ensure a continuous laminar airflow or Grade A air environment is maintained.
 Figure 3 Filling machine equipment
Figure 3 Filling machine equipment
7. Addressing Challenges in Complex Manufacturing Systems
 Figure 4 Complex manufacturing system with multiple vessels, CIP and SIP skids and numerous connections
Figure 4 Complex manufacturing system with multiple vessels, CIP and SIP skids and numerous connections
In complex manufacturing systems (see Figure 4) that involve multiple vessels, clean-in-place (CIP), SIP skids, and numerous connections, addressing specific challenges is crucial to prevent media fill failures. This includes ensuring robust sterilization, validating SIP processes, conducting water trials, and performing comprehensive leak tests for the entire system. Attention should be given to the placement of sensors, temperature validation, and smoke studies to confirm the system's integrity. Skipping essential steps such as water trials or conducting leak tests after interventions can lead to unexpected issues during media fill.
Conclusion
Investigation of media fill can be effectively done by following strategies such as tabulating activities, establishing connections between activities and contamination, and addressing factors like environmental conditions, equipment assembly, and cleaning procedures. In addition, manufacturers can identify the root cause of failures and implement corrective actions and preventive actions to ensure product safety and prevent contamination in sterile products.



 Niravbhai Patel, PhD, has a rich history of leading teams for approximately two decades in the creation of the U.S. FDA applications for various types of products, including brand, generic, sterile, and
combination products. Niravbhai leadership skills have been instrumental in conducting due diligence for licensing opportunities and managing crucial partnerships, all while utilizing his expertise in pharmaceutical development, project management,
and leadership. Patel's notable achievements include successfully bringing a multitude of 505(j) and 505(b)(2) applications to the market, collaborating with various functions from research and development to business development, and offering
strategic insights on product in-licensing and acquisitions. At present, Patel holds a leadership position at Nivagen Pharmaceuticals, Inc.
Niravbhai Patel, PhD, has a rich history of leading teams for approximately two decades in the creation of the U.S. FDA applications for various types of products, including brand, generic, sterile, and
combination products. Niravbhai leadership skills have been instrumental in conducting due diligence for licensing opportunities and managing crucial partnerships, all while utilizing his expertise in pharmaceutical development, project management,
and leadership. Patel's notable achievements include successfully bringing a multitude of 505(j) and 505(b)(2) applications to the market, collaborating with various functions from research and development to business development, and offering
strategic insights on product in-licensing and acquisitions. At present, Patel holds a leadership position at Nivagen Pharmaceuticals, Inc. Dhavalkumar Surti has over 20 years of experience in injectable manufacturing, validation, quality assurance, and new facility projects. From 2003, Surti worked with reputable companies like Reddy’s,
PhD, Sun Pharmaceuticals, Zydus Pfizer Oncology, Emcure Pharmaceuticals, and Aculife Healthcare. Surti has core experience in aseptic technique, freeze drying, sterilization validation, media fills, smoke studies, SOP writing, investigations,
and training. Currently, Surti holds a lead validation/qualification sterile manufacturing position at Nivagen Pharmaceuticals, Inc.text
Dhavalkumar Surti has over 20 years of experience in injectable manufacturing, validation, quality assurance, and new facility projects. From 2003, Surti worked with reputable companies like Reddy’s,
PhD, Sun Pharmaceuticals, Zydus Pfizer Oncology, Emcure Pharmaceuticals, and Aculife Healthcare. Surti has core experience in aseptic technique, freeze drying, sterilization validation, media fills, smoke studies, SOP writing, investigations,
and training. Currently, Surti holds a lead validation/qualification sterile manufacturing position at Nivagen Pharmaceuticals, Inc.text