An Uncommon Battle: Living with Chronic Intestinal Pseudo-Obstruction
The 2023 PDA Annual Meeting in New Orleans, April 3-5, was filled with over 300 hundred industry members who came together and reported changes happening in pharma. Monday through Thursday consisted of noteworthy sessions that centered around leaders in the industry, such as scientists and regulators who shared their perspectives on topics regarding the revision of European Union Annex 1: Manufacture of Sterile Medicinal Products, the blooming acceleration of achieving cybersecurity in healthcare and the steps that are actively being pursued in the industry that are pushing the boundaries for new drug development.
Meeting Kelly Baker
The first plenary session on day one of the annual meeting set the tone for the rest of the informative sessions throughout the 2023 PDA Annual Meeting.
After the introductions from Susan Schniepp (Board of Director’s Chair), Glenn Wright (PDA’s President and CEO), Amanda McFarland (Senior Consultant, ValSource, Inc) and Julia Jenkins (Executive Director, EveryLife Foundation for Rare Diseases), Kelly Baker (rare disease representative) took center stage to talk about a rare disorder called chronic intestinal pseudo-obstruction (CIPO).
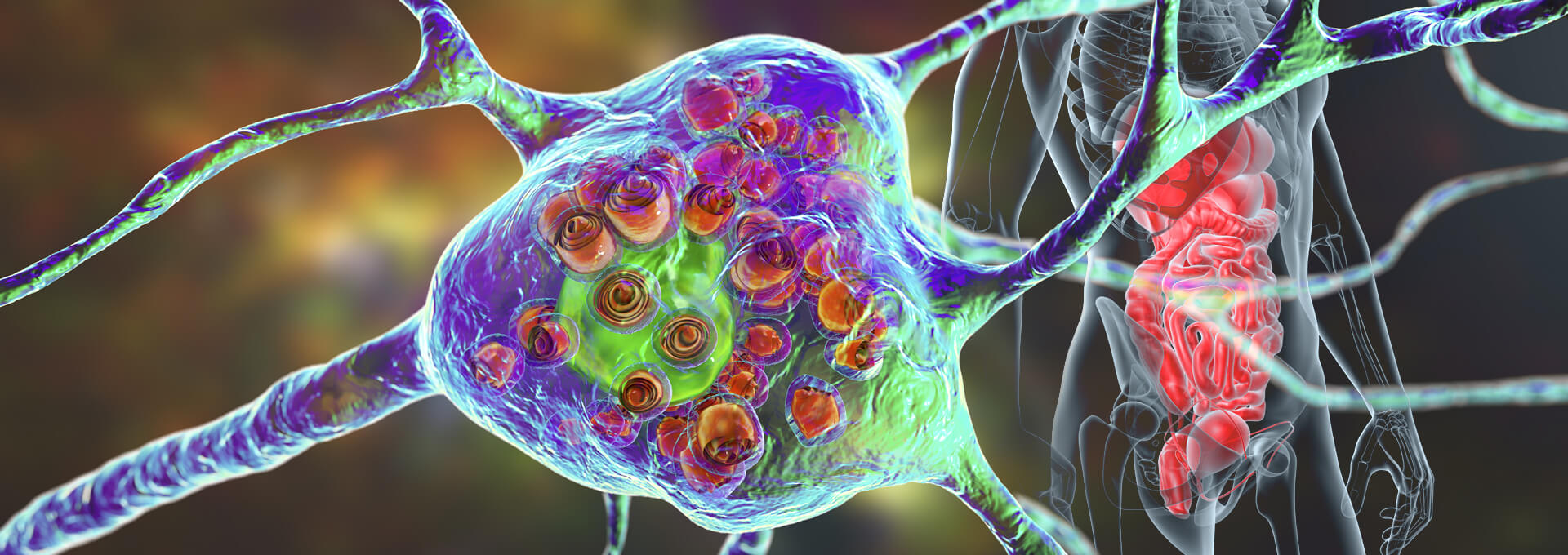
According to the National Institutes of Health (NIH), CIPO is a lifelong, rare motility disorder found in children that causes abnormalities in the nerves, muscles, or both, preventing food, fluid and air from moving through the stomach and intestine, which cause mechanical obstruction or blockage. In addition, CIPO can occur as a primary condition called idiopathic CIPO or as a secondary condition associated with underlying diseases such as autoimmune disorders, neurological conditions, connective tissue disorders, or certain medications. As it pertains to diagnosing CIPO, the NIH’s studies have shown that it can be difficult, given that it requires subtracting other potential causes of intestinal obstruction and evaluating motility patterns in the gastrointestinal (GI) tract. Diagnostic tests may involve imaging studies (such as X-rays, ultrasound, or computed tomography), manometry (measuring muscle contractions in the intestine) and endoscopy to visualize the intestines directly. Moreover, treatment for CIPO aims to manage symptoms, improve motility and prevent complications. It typically involves a multidisciplinary approach involving gastroenterologists, nutritionists and other specialists. Nonetheless, the Boston Children’s Hospital expounds on the most common treatments of CIPO that assist in controlling symptoms or complications, which include the following:

- Medicine or symptom management: Different medications can be prescribed to regulate intestinal motility, control symptoms like pain and nausea and manage complications such as bacterial overgrowth. These medications usually include oral medicines and epidural anesthesia.
- Nutrition support: Nutritional deficiencies are common in CIPO, and individuals may require specialized diets or nutritional supplements to ensure adequate nutrient intake. Some doctors may recommend parenteral nutrition, which supplies nutrients directly into the veins using a catheter.
- Surgery: In some severe cases, surgery to remove part of the intestines might be necessary, known as surgical decompression. A surgeon may insert a feeding tube directly into the stomach or create an opening in the abdomen through which the intestines can release gas and empty stool, causing pressure to be released from the intestines. In some patients, when pseudo-obstruction is limited to an isolated segment of the bowel, surgical bypass may be considered. However, this procedure is usually the last resort and is not always effective.
After Kelly’s presentation, everyone in the room stood and applauded Kelly for her bravery in speaking about her condition, along with the grit she possesses to live with a lifelong disease that causes frequent abdominal pain.
“That brave young lady who talked about her experience with CIPO is why we are here today and is why we care about science,” said Vinicius Tarantino (Head of Digital Compliance and Protection, GXP-CC) during his session on cybersecurity and risk management at the 2023 PDA Annual Meeting, and a majority of other members at the annual meeting felt that exact sentiment throughout the conference.
[Following the conference, the Managing Editor of the PDA Letter interviewed Kelly regarding her experience with CIPO.]
PDA Letter: Considering the standing ovation you received after your presentation at annual, do you see any urgency or effort in the pharmaceutical industry to find better treatment for CIPO?
Kelly: I appreciate the support from the audience after my presentation. However, I realize that progress in the pharmaceutical industry can take time, especially when it comes to drug development, policy and manufacturing. Currently (and for the past few years), there is not much research or drug/treatment development happening for CIPO.
The main treatment for CIPO is symptom management, which sometimes includes parenteral medications and nutrition. I would like the pharma industry to realize the impact of drug shortages and access concerns for patients like me who rely on these products to live.
PDA Letter: When were you diagnosed with CIPO? And was your diagnosis primary or secondary? Also, what are some personal challenges that you have experienced with this disease?
Kelly: For the first part of that question. From birth, I was pretty much a healthy kid with only mild GI problems that did not affect my life. However, around twelve, my disease worsened to needing a feeding tube. Then after a couple of years on the feeding tube, my CIPO worsened, causing me to go on total parenteral nutrition (TPN). I have been on TPN ever since, but I have periods where my condition is better. It is common for CIPO patients to have episodes of worsening symptoms and periods that are better. I have fewer symptoms during my better periods and can tolerate more through my feeding tube and orally, but I still need TPN. Some CIPO patients on TPN can get enough enteral/oral intake during better periods to decrease their TPN needs.
Now, for the second part of the question. I do not know how common it is to be diagnosed with a specific type of CIPO, but I fall somewhere in the middle. My case could be considered secondary because I have a connective tissue disease (Ehlers-Danlos syndrome) that may have caused the CIPO. Still, due to the severity, it could also be a separate condition that could list it as primary. Unfortunately, the type of CIPO does not affect treatment since there are not yet any treatments or research specific to a particular type of CIPO.
PDA Letter: What advice would you give to young people who might also be suffering from CIPO? What are some treatments that you use for this disease?
Kelly: Connecting with other people who have CIPO in person or online through social media can be really helpful and allows you to get support from others who have been through or are going through similar things. Having a life-long disease is hard, but educating yourself on your condition and finding support can empower you and increase your confidence in advocating for your medical care. At first, it may feel like your world revolves around your disease, but over time you will adjust to your “new normal” and find ways to cope. Finding passions, interests and hobbies outside of your illness is also an important outlet for emotions and creativity that can help increase motivation.
PDA Letter: You mentioned individuals with CIPO, over time, will adjust to their “new normal. How do you keep the motivation to live life normally? What does a normal life look like to you?
Kelly: Well, since I have a life-long disease, I really have no choice but to live my life as “normally” as possible. Some days are harder than others, and it can be difficult to be optimistic when my pain/nausea is severe. When you have a condition such as mine, you learn the importance of radical acceptance or accepting that you cannot change your situation but can change your perspective and move forward. You do not have to have a positive attitude or be optimistic about having a difficult illness, but acceptance helps you focus on what you can change about your situation. My interest in medicine and public health advocacy motivates me to continue working toward my goals even during periods of worse illness.
A New Hope Moving Forward
PDA Letter: Now that it has been a couple of months since the 2023 PDA Annual Meeting, how has life been after attending the meeting? What is next for you?
Kelly: Immediately after the conference, I had a few people reach out to me to discuss how rare diseases have affected their lives through friends/family members as well as questions about living on parenteral nutrition. I have not gotten many opportunities to spread awareness since then (other than now), but I truly appreciate the opportunity I was given to speak at the annual meeting.
I am currently working on my degree in nursing, and I would like to continue doing public speaking to educate and spread awareness. I also have had an opportunity to be a patient/consumer reviewer for a scientific research panel that I enjoyed, and I would love to be more involved in research.
Conclusion
PDA has invited patients of serious illnesses to present at its conferences for many years. These presentations continue to serve as affirmation of the important work our members perform as a critical cog in the machinery that produces lifesaving and life-altering therapeutic medicines. PDA thanks Kelly for sharing her story at the 2023 PDA Annual Meeting and for participating in this follow-up interview.


