A supplier's perspective: How can EU GMP Annex I be integrated into the manufacturing of components for container closure systems?
Suppliers of primary packaging components can make a significant contribution to pharmaceutical manufacturers’ efforts to comply with EU GMP Annex I, maintain quality, and reduce product and patient risk, by aligning with Annex 1 throughout the component manufacturing process, where applicable.
Annex I: Manufacture of Sterile Medicinal Products was first developed in 1971 and experienced its latest big revision attempt in 2018. This revision was so significant that it is still ongoing but expected to be published early 2022. The revision process was a collaborative effort with the World Health Organization (WHO) and the Pharmaceutical Inspection Co-operation Scheme (PIC/S). Through PIC/S, the U.S. FDA and an additional 53 authorities from all over the world are now included.
The content has been updated and the structure reorganized in a way to be aligned with globally accepted standards and recommendations.
The most significant addition is the focus on a formal, holistic contamination control strategy. The expectation now appears to be for a formal document that reflects the site-wide strategy for minimizing contamination, such as particulates, microbes, and pyrogens throughout the whole sterile manufacturing process. Another focus is on the introduction of new technologies, such as Restricted Access Barrier Systems (RABS) and isolators which are strongly encouraged to be built into the facility upgrade.
On the container closure side, more attention has been given to an in-depth understanding of container closure integrity (CCI). Highly debated is the 100% integrity testing for containers closed by fusion as it is not yet clear how this can be implemented in the real-time manufacturing process.
Finally, the current revision embraces the philosophy of a holistic risk management system. The latest draft contains many references to Quality Risk Management (QRM) in particular, emphasizing that QRM should be used as a proactive tool and thus establishing the connection to the globally accepted and enforced International Council for Harmonisation (ICH) of Technical Requirements for Pharmaceuticals for Human Use (ICH) Q9 (Quality Risk Management) and Q10 (Pharmaceutical Quality System).
The expected benefit from this is fewer deviations in manufacturing and an improved supply chain integrity.
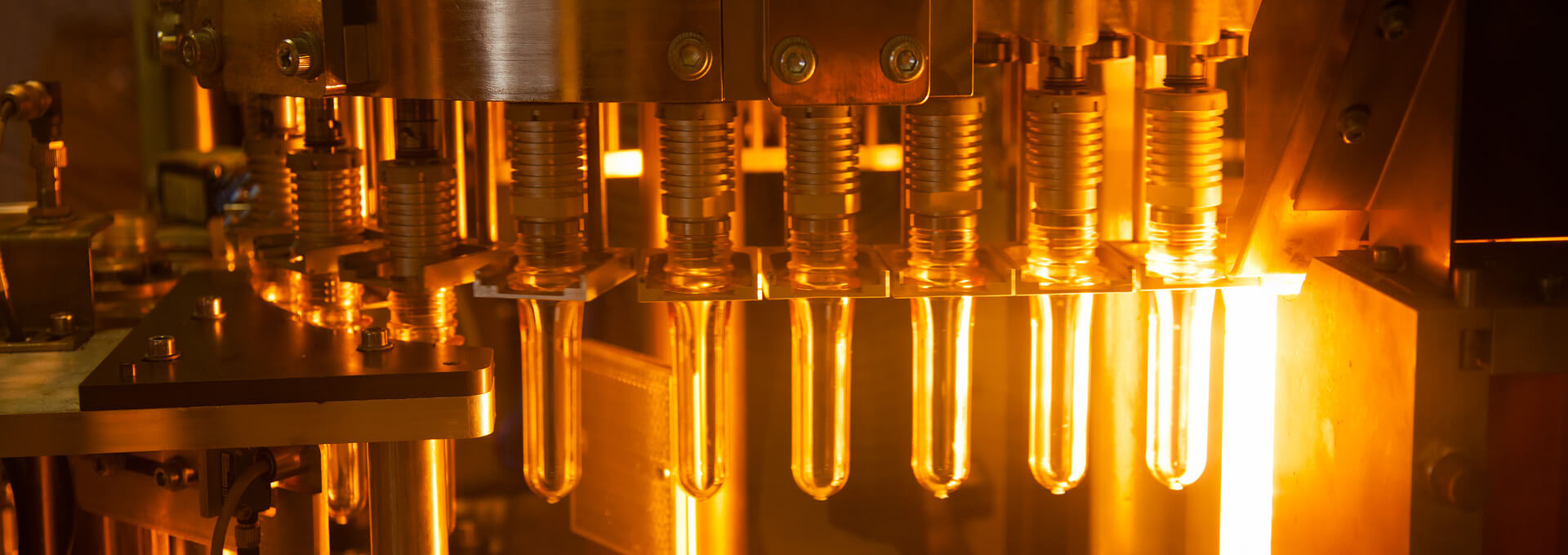
Due to its high relevance, in the past years, there have been numerous presentations, discussions and publications related to the manufacturing of the drug product, but rather less focus on the primary packaging components. As they are starting material, it is equally important to ensure that they don’t introduce uncontrolled levels of microbial, particulate and pyrogen contamination.
This article will provide a suppliers’ perspective of how the principles of EU GMP Annex I can be integrated into the manufacturing of sterile primary packaging components.
Quality Management System (QMS)
According to EU GMP Annex I, a functional quality system is the base to ensure that all activities are effectively controlled. Chapter 3 highlights the specific requirements of the pharmaceutical quality system when applied to sterile products.
A supplier having multiple manufacturing sites should have a quality system that is managing processes both on a global and a site-specific level to account for the individual regional circumstances and requirements. Depending on the products that are manufactured, these sites should possess current certificates, such as:
- ISO 9001 — Quality management systems – Requirements
- ISO 15378 — Primary packaging materials for medicinal products. Particular requirements for the application of ISO 9001:2015, with reference to good manufacturing practice (GMP)
- ISO 13485 — Medical devices – Quality management systems – Requirements for regulatory purposes
The global quality system approach should be described in a quality manual which contains the scope of the quality management system and its realization through different elements. These elements can be prescribed in the quality policy/requirements, standard operating procedures and work instructions, based on International Organization for Standardization (ISO) standards, current regulatory requirements, industry guidances, and good manufacturing practices (GMPs). The quality manual should be communicated through all levels of the company and reviewed periodically for continuing effectiveness.
The work instructions identify the relevant processes to comply with applicable regulatory and customer requirements and standards, outline the management responsibilities within the quality system, contain descriptions on process performance and product quality monitoring, corrective and preventive action, change management and management review. Furthermore, they include an effective quality risk management which is integrated into all areas of the product lifecycle for identifying, scientifically evaluating and controlling potential risks to quality and thus facilitate continual improvement of process performance and product quality throughout our product lifecycle.
Science and risk-based approaches should be used to define performance indicators of the quality system and to meet the appropriate quality attributes for all products.
ISO 14644 Cleanroom Classifications
EU GMP Annex I cleanroom classification is consistent with current ISO 14644-1:2015 standard for cleanroom Classification of Air Cleanliness by Particle Concentration. A specific focus was set on removing the ≥ 5 μm particles limit for ISO Class 5. To ensure consistency, all global manufacturing plants should be aligned with the current ISO 14644-1:2015 standard for cleanroom Classification of Air Cleanliness by Particle Concentration. The respective standard operating procedures should be set and be in alignment with the quality manual.
Contamination Control Strategy
A deliberate and well-documented contamination control strategy is one of the new focuses in the Annex I document. The main additions and revisions are in 2.1. “The manufacture of sterile products is subject to special requirements in order to minimize risks of microbial, particulate and pyrogen contamination.” and in 8.2 “Primary packaging containers and components should be cleaned using validated processes to ensure that particulate, pyrogen and bioburden contamination is appropriately controlled.”
Depending on the quality level, a specification for particles should be set in place. The measurement methods should be in accordance with ISO 8871-3 and European Pharmacopeia (Ph. Eur.) 2.9.19.
For pyrogens such as endotoxins, additional special controls for cleaning equipment and tooling, water and filtration system should be in place. The pharmaceutical washing process should be a validated process with a defined cycle per item, which results in product that meets specified limits for bacterial endotoxin, bioburden, particulate matter and, if applicable, silicone oil level. The process validation study data should demonstrate that the pharmaceutical washing process is capable of reducing the endotoxin content by at least 99.9% (3.0 log10).
According to 10.4 “A pre-sterilization bioburden monitoring program for the product and components should be developed to support parametric release. The bioburden should be performed for each batch.” Thus, the pharmaceutical washing process should ensure a low bioburden level which should be controlled on a batch-release basis.
All relevant information should be stored in Drug Master Files (DMF) with the US FDA and Health Canada. The used water system should be fully qualified and the qualification reports on file at the applicable sites.
After washing, the primary packaging components should be unloaded and packed into appropriate bags, e.g., in an ISO 5 (particle limits ISO 5 ‘in operation’) clean room prior to shipment.
A globally harmonized, validated method to determine endotoxin concentration, which conforms with USP <1228>, USP <85>, USP <161>, Ph. Eur. 2.6.14. and ANSI/AAMI ST72:2011 should be in place.
According to 10.5 “The sterility test applied to the finished product should only be regarded as the last in a series of control measures by which sterility is assured. It cannot be used to assure sterility of a product that does not meet its design, procedural or qualification parameters. The test should be validated for the product concerned.” The supplier should have a contamination control strategy for its manufacturing environment in place which should be embedded in the quality management system and in line with the quality manual. It should refer to the minimization of the risk on the primary packaging components of contamination from particulate and microbial sources, including pyrogens such as endotoxins. It should be controlled on a site level and specified in a series of different events and measures written down in the respective standard operating procedures.
Areas within the process controls include but are not limited to incoming raw materials, in-process materials, tooling, line clearance procedures, gowning requirements, cleanroom and general environmental controls.
According to 10.10 “Environmental monitoring data and trend data generated for classified areas should be reviewed as part of product batch certification.” On-going monitoring of product and process data should be tracked within the quality system. Periodic review, process monitoring, and focused studies should be undertaken with the intent of supplementing the overall control strategy.
Methods used to monitor the continued performance of the systems should be executed following a certain methodology. Monitoring frequency, alert and action limits should be described in procedures on file at the site. The used water system should be tested daily for bacterial endotoxin levels, total organic carbon, conductivity and bioburden. At specified intervals, the incoming water should be tested for coliform bacteria.
Based on the suppliers thorough technical knowledge and in-depth knowledge of the processes, if required, procedures should be actively updated and driving continuous improvement of the manufacturing and control measures.
Steam and Gamma Sterilization Process
According to section 2.7 of EU GMP Annex I, “Sole reliance for sterility or other quality aspects should not be placed on any terminal process or finished product test”. This refers to the pharmaceutical manufacturing process. However, as elastomeric components are increasingly delivered in a sterile format, they need to be considered as well. Regardless of whether the sterilization is performed in-house or with an external partner, the processes need to be validated and documented.
All pertinent equipment and facilities should be qualified. Processes should be validated and controlled and are based on scientific principles and data which demonstrate repeatability and reliability of the sterilization program. Critical parameters (such as time, temperature and pressure) are defined, controlled, monitored and recorded. The unloading of the autoclave should take place in a controlled environment, e.g., ISO 7 in operation clean room. These same details of the steam sterilization process should be filed in a DMF with US FDA and Health Canada.
Additionally, in-house steam sterilization sites should be FDA registered and hold a statement of conformance to ISO17665-1:2006 Sterilization of Healthcare products – Moist Heat Part 1. The validation approach should utilize a half cycle validation method in which Biological Indicators are used based on ISO 17665-1 and ISO 17665-2 Sterilization of Healthcare Products – Moist Heat to demonstrate appropriate kill at established validated cycle parameters.
The steam sterilization process should be validated to achieve a Sterility Assurance Level (SAL) of 10-6 or better. All steam sterilization half cycles should meet the acceptance criteria (including temperature ranges and accumulated lethality) set forth in the validation protocols. Sterilization process validation should be maintained through appropriate change control and revalidation/periodic review programs all of which comply with applicable current GMP (cGMP) requirements.
Validation studies should be performed using a bracketing approach for the sterilization process and packaging systems. Package format, configuration and fill quantity, total autoclave load mass, component formulation and formulation bioburden resistance are used as criteria to evaluate whether a component format falls within the established process range.
Referring to 8.54 the sterilized items should be inspected for damage, seal and packaging material integrity and moisture on removal from the autoclave.
The gamma sterilization validation should be performed according to the current ANSI/AAMI/ISO 11137 Sterilization of health care products – Radiation Part 1, 2 and 3.
Portbags
According to section 4.18 of EU GMP Annex I, “The entry of materials during processing (and after decontamination) should be minimized and preferably supported by rapid transfer technologies or transfer isolators.”
Annex I clearly supports a facility upgrade to using barrier technologies, such as isolators and RABS. For material transfer into these systems elastomer and seal components are typically supplied in aseptic transfer single-use portbags equipped with a beta port that are compatible with the corresponding alpha ports.
The available portbag options should be verified to meet incoming inspection criteria for bioburden, endotoxin and particulates. They should allow for sterility assurance using the above-mentioned steam sterilization process. Sterile barrier integrity should be maintained throughout the whole packaging, sterilization and transportation process and should be proven to conform with ISO 11607 Packaging for Terminally Sterilized Medical Devices. The testing should include visual assessments of bag seals (American Society for Testing and Materials (ASTM) F 1886), leak detection using internal pressurization (ASTM F 2096) and dye testing (ASTM F 1929) if required to confirm a suspected seal area during visual inspection or internal pressurization. Packaging post-sterilization shelf-life studies should be performed to ensure sterilized samples meet sterile barrier integrity throughout the entire shelf life. Packaging design verification studies should be conducted to demonstrate the maintenance of sterile barrier integrity through the stresses imposed by packaging, sterilization and transport simulation for unitized load (pallet) distribution per ASTM D 4169-05 Standard Practice for Performance Testing of Shipping Containers and Systems.
Conclusion
To support pharmaceutical manufacturers’ compliance with EU GMP Annex I, to maintain quality, and reduce product and patient risk, suppliers of primary packaging components can make a significant contribution. Where applicable, alignment throughout the component manufacturing process with the important philosophies and requirements of Annex I represent the first step. This article highlighted the areas where this alignment can be achieved.



 As Principal of Scientific Affairs, Bettine Boltres, PhD, supports the scientific exchange between West Pharmaceutical Services and the pharmaceutical industry. She is also a volunteer PDA Director.
As Principal of Scientific Affairs, Bettine Boltres, PhD, supports the scientific exchange between West Pharmaceutical Services and the pharmaceutical industry. She is also a volunteer PDA Director.